Abstract
Introduction: Characterization of molecular landscape in acute myeloid leukemia (AML) leads to update of known prognostic classifier or to create new ones. We analyzed the prognostic impact of ELN 2017 (Döhner et al., Blood 2017), ELN 2022 (Döhner et al., Blood 2022), ALFA classifier (Itzykson et al. Blood 2021), Lindsley classifier (Lindsley et al. Blood 2015) and Papaemmanuil classifier (aml-risk-model.com/calculator) in a large cohort of AML adult patients.
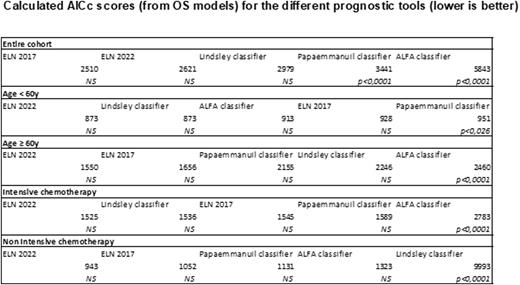
Methods: In this monocentric study (Nice University Hospital), the prognostic scores were calculated using all five risk stratification models (ELN 2017, ELN 2022, ALFA classifier, Lindsley classifier and Papaemmanuil classifier) and risk categories were determined for each adult patient treated for an AML between January 2015 and January 2022. Overall survival (OS) was calculated from the time of diagnosis of AML to the time of death or last known follow-up. Median OS was estimated using the Kaplan−Meier method, and differences between subgroups were assessed using the log-rank test. Cox proportional hazards models were fit to assess association of prognostic systems with OS. Corrected Akaike Information Criteria (AICc) were used to compare these fitted models.
Results: Two hundred ninety consecutive AML patients treated in our institution were included from 2015 to 2022. Median age was 68 years old (18-93, range). Sex ratio M/F was 160/125. Performans status was ≤ 2 in 93% of patients. AML were de novo in 74%, therapy related in 5%, secondary in 21%. Intensive chemotherapy, non-intensive chemotherapy and best supportive care were used in 53%, 40% and 6% of patients, respectively. ELN 2017, ELN 2022, ALFA classifier, Lindsley classifier and Papaemmanuil classifier were calculated in 96%, 99%, 87%, 88% and 93% of patients, respectively.
With a median follow up of 7.9 months (0-78, range), median OS in the entire cohort was 40.2 months (95% CI, 14.6-65.9). We observed significant differences using ELN 2017 (Favorable : 83.3 months / Intermediate : 40.2 months / Adverse : 12.4 months, p<0.0001) ; ELN 2022 (Favorable : 83.3 months / Intermediate : 43.2 months / Adverse : 9.2 months, p<0.0001) ; ALFA classifier (Go go : 83.3 months / Slow go : 34.7 months / No go : 9.5 months, p<0.0001) ; Lindsley classifier (De novo/pan AML : 83.3 months / Secondary : 13.3 months / TP53 mutated : 10.1 months, p<0.0001) and Papaemmanuil classifier (Favorable : 83.3 months / Intermediate : 40.2 months / Adverse : 10.7 months, p<0.0001).
The AICcs were used to compare the univariable Cox models containing prognostic scoring systems as covariates (lower is associated to a better prediction). The AICcs for the OS models were 2510 (ELN 2017), 2621 (ELN 2022), 2979 (Lindsley classifier), 3441 (Papaemmanuil classifier) and 5843 (ALFA classifier) (Table). ELN 2017, ELN 2022 and Lindsley classifier were significantly better in the entire cohort of treated AML patients. To assess if the relative prognostic discrimination for the five prognostic tools was influenced by age or type of treatment, we calculated the AICc scores for the five prognostic tools in each of these subgroups (Table). We observed a trend for a better stratification of patients with ELN 2022 in age < or ≥ 60 years old and in patients treated with intensive and non-intensive chemotherapy. In our cohort, Papaemmanuil and ALFA classifier were significantly less suitable for stratification in younger patients (< 60 years old) (p=0.026) and in patients treated intensively (p<0.0001), respectively. ALFA classifier was significantly less suitable for stratification in patients treated by intensive chemotherapy (p<0.0001). Lindsley classifier was significantly less suitable for stratification in patients treated by non-intensive chemotherapy (p<0.0001).
Conclusions: Among all risk stratification tools available in AML, ELN 2022 seems to be the best prognostic score in younger and older patients independently of the received treatment. These observations need to be validated in a larger cohort.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal